Written and medically reviewed by Rich LaFountain, PhD
BMI, or body mass index, is at its core, a health-screening tool. With simple inputs of height and weight, this tool has been used for decades as a quick indicator of physical health and, importantly, risk of chronic disease.
We know from data on people who live to be 100 or older that one of the best ways to extend your lifespan is to prevent chronic disease. People don’t usually manage to live extremely long lives when they’re riddled with disease; those who live for over a century are able to delay disease and can thereby maintain independence into their eighth and ninth decade of life.
Ultimately, if you can delay disease, you’re likely to live longer. That means it’s important to identify — and then mitigate — risk of disease. Helping identify that risk is how and why BMI became popular.

The Body Weight Debate
Today BMI is accepted as the international standard metric for classification of health based upon body weight. However, that wasn’t always the case. For almost two hundred years clinicians, researchers, and even insurance agents have debated what it means to have a “healthy body weight.” Quetelet’s index, the original name for BMI, was Lambert Adolphe Jacques Quetelet’s answer to that debate. He developed and published his index in 1835, although it was not widely used until the 1970s.
BMI for Longevity
Unlike direct body weight measures in pounds or kilograms, BMI uses body height to normalize body weight. This is an important distinction, because a weight of 200 lbs can have very different health implications for a person who is 5’3” compared to someone who is 6’3”.
BMI works by classifying people into risk groups based on their normalized weight. To see where you fall, you can calculate your BMI by hand (body mass index = body weight in kg ÷ height in m2) or by using one of many free online calculators or app features. A BMI of 21-25 kg/m2 is considered “normal” or “healthy.”
What’s important to know from a longevity standpoint is that in large, long-term studies, adults who fall within this “healthy” BMI range and whose weight stays stable over time also have the lowest disease and mortality risk. In a nutshell, life expectancy and disease-free healthspan are on average 7 years longer in women and 9 years longer in men who maintain stable healthy BMI throughout their adult lives. Considering how important it is to delay the onset of chronic disease if we want to live longer, BMI gives us a range to shoot for that can help us maximize our genetic lifespan potential.
Why Does Body Weight Matter?
Abundant research data demonstrate a clear link between BMI, disease risk, and all-cause mortality. However, despite what diet-culture media may have you believe, the relationship is not linear. A j-curve relationship illustrates that humans with very low or very high BMI have higher risk. In a 2018 study that included over 3.5 million people, researchers found that being underweight (BMI <18.5kg/m2) or obese (BMI >30kg/m2) was associated with a 3.5-4.5-year reduction in life expectancy. Thus, BMI definitely can serve as an indicator of longevity potential in most adults, but it is not perfect, and it’s certainly not the only thing that matters.

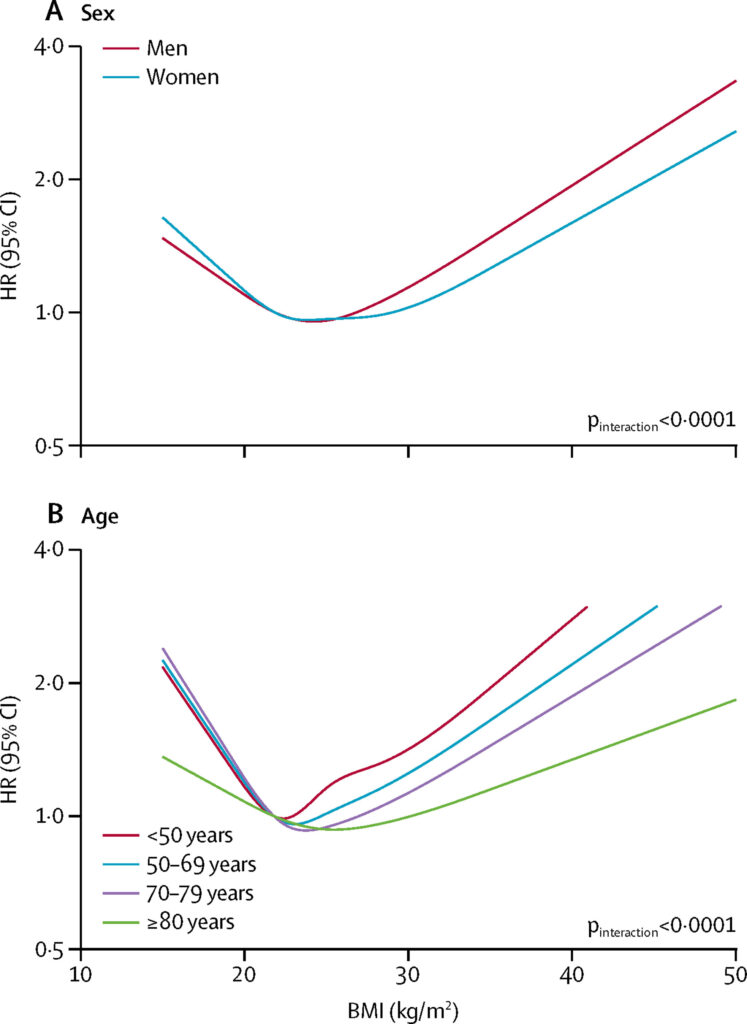
BMI and Aging
One factor that matters and which BMI does not account for is age. As we age, our risk of disease and infection gradually grows, and the BMI that is best associated with longevity may shift, as well. Recent evidence supports increasing the target BMI range for adults over age 65. A meta-analysis from 2014 concluded that older participants with BMI of 26-28.9 kg/m2 (as opposed to the standard “healthy” range of 21-25 kg/m2) minimized mortality risk. Several hypotheses describe why this may be the case: for example, higher BMI may provide older adults with more stored energy to combat illnesses or protect them from injuries which may otherwise be life-threatening.
Other Limitations
Although BMI is the current broad standard and can provide us insight on physical health in the general population, BMI unfortunately does not always serve individual humans well. While BMI is normalized by height, it does not account for individual differences in muscle or fat mass. As a result, BMI often misclassifies athletes who have increased muscle mass (which increases their weight but not their risk of chronic disease or death). In addition, BMI does not classify people equally across diverse groups because it was not created in a representative sample. (Quetelet created it using — as most researchers of his time did — the measurements of white Western Europeans.)
In addition, and probably most importantly, BMI does not provide any direct information about metabolism. Research demonstrates that many people with a BMI >30 kg/m2 (which the CDC classifies as obese) can can also be metabolically healthy. Metabolically healthy obese individuals have lower risk and higher longevity potential across their lifespan than normal weight metabolically unhealthy individuals. Put another way, metabolic health matters more than weight when it comes to healthspan and lifespan.
BMI certainly isn’t perfect, as metabolic health is also clearly essential for assessing overall health and longevity. That said, BMI is superior to its “ideal body weight equation” predecessors. BMI is also less complicated (and less expensive) than measuring body composition, which requires specialized equipment, equations, and training. For most adults striving to extend healthspan and lifespan, BMI is an accessible way to assess health risk in relation to their body weight. This makes BMI a valuable tool for pursuing better health and longevity.
References
Sebastiani, P., & Perls, T. T. (2012). The genetics of extreme longevity: lessons from the new England centenarian study. Frontiers in genetics, 3, 277.
Pignolo R. J. (2019). Exceptional Human Longevity. Mayo Clinic proceedings, 94(1), 110–124.
Hitt, R., Young-Xu, Y., Silver, M., & Perls, T. (1999). Centenarians: the older you get, the healthier you have been. Lancet (London, England), 354(9179), 652.
Czerniawski, A. M. (2017). a 200-year weight debate. Contexts, 16(3), 68-69.
Sorkin J. D. (2014). BMI, age, and mortality: the slaying of a beautiful hypothesis by an ugly fact. The American journal of clinical nutrition, 99(4), 759–760.
Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J., & Smeeth, L. (2018). Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. The lancet. Diabetes & endocrinology, 6(12), 944–953.
Abernathy, R. P., & Black, D. R. (1996). Healthy body weights: an alternative perspective. The American journal of clinical nutrition, 63(3 Suppl), 448S–451S.
Stenholm, S., Head, J., Aalto, V., Kivimäki, M., Kawachi, I., Zins, M., Goldberg, M., Platts, L. G., Zaninotto, P., Magnusson Hanson, L. L., Westerlund, H., & Vahtera, J. (2017). Body mass index as a predictor of healthy and disease-free life expectancy between ages 50 and 75: a multicohort study. International journal of obesity (2005), 41(5), 769–775.
Global BMI Mortality Collaboration, Di Angelantonio, E., Bhupathiraju, S., Wormser, D., Gao, P., Kaptoge, S., Berrington de Gonzalez, A., Cairns, B. J., Huxley, R., Jackson, C., Joshy, G., Lewington, S., Manson, J. E., Murphy, N., Patel, A. V., Samet, J. M., Woodward, M., Zheng, W., Zhou, M., Bansal, N., … Hu, F. B. (2016). Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet (London, England), 388(10046), 776–786.
Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J., & Smeeth, L. (2018). Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. The lancet. Diabetes & endocrinology, 6(12), 944–953.
Andres R. (1980). The obesity-mortality association: where is the nadir of the U-shaped curve?. Transactions of the Association of Life Insurance Medical Directors of America, 64, 185–197.
Winter, J. E., MacInnis, R. J., Wattanapenpaiboon, N., & Nowson, C. A. (2014). BMI and all-cause mortality in older adults: a meta-analysis. The American journal of clinical nutrition, 99(4), 875–890.
Tomiyama, A. J., Hunger, J. M., Nguyen-Cuu, J., & Wells, C. (2016). Misclassification of cardiometabolic health when using body mass index categories in NHANES 2005-2012. International journal of obesity (2005), 40(5), 883–886.
Nuttall F. Q. (2015). Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutrition today, 50(3), 117–128.
Rahman, M., & Berenson, A. B. (2010). Accuracy of current body mass index obesity classification for white, black, and Hispanic reproductive-age women. Obstetrics and gynecology, 115(5), 982–988.
Blüher M. (2020). Metabolically Healthy Obesity. Endocrine reviews, 41(3), bnaa004.
Du, T., Fonseca, V., Chen, W., & Bazzano, L. A. (2022). Changes in body size phenotypes from childhood to adulthood and the associated cardiometabolic outcomes. Diabetes research and clinical practice, 187, 109884. Advance online publication.
- Debunking 3 Myths Around Fasting and Thyroid Health - April 15, 2024
- Breaking Down Fast Breakers: How to Tell If Something Will Break Your Fast - March 4, 2024
- GLP-1s and Weight-Loss Medications vs. Lifestyle Interventions: What’s Right for You - February 5, 2024