Written and medically reviewed by Rich LaFountain, PhD
By: Rich LaFountain
My Introduction to Fasting – The Prolonged “Hospital Fast”
My first year in graduate school, during spring break, I had lower right quadrant pain in my abdomen. My stomach hurt, but it wasn’t a traditional stomach ache. It was the kind of stomach ache that makes it difficult to stand up straight. After a few days, the pain seemed to get more intense. I finally drove to the hospital in the middle of the night, but somewhere along the drive the pain seemed to subside, so naturally I drove home and went back to bed. Several hours later, it was back with a vengeance. I went back to the hospital and checked into the emergency department with what I believed was appendicitis. After some ultrasounds and a CT scan it was determined I had an inflamed Meckel’s Diverticulum and this sneaky congenital deformity would have to be removed right away. Following a resection of my small bowel I became an in-patient and was required to “fast” for about 7 days. I use the term “fast” in quotations because I am fairly certain I received IV glucose infusion during my time in the hospital. Thinking back on it now, I am discouraged at the thought that I may have had sugar mainlined directly into my blood!
Eventually I graduated to solid food and was cleared to leave the hospital. Although it was suggested I would have an elevated probability of bowel obstructions following surgery, there was little information shared pertaining to diet changes that might mitigate my risk.
Two years later, wouldn’t you know it, I had a small bowel obstruction. This again landed me in the hospital where the treatment options were 1) surgery or 2) stop food consumption and “unpack” from the top side using a nasogastric (NG) tube and fluid infusion for several days until the problem cleared up. I opted for option 2. The whole process took about 7 days. This experience with hospital “fasting” was even worse than my first for several reasons. This time it was not spring break, I was missing work, school, and teaching. I also had at least 2-3 days of being fully awake to experience the incredible discomfort of the NG tube. Whereas, post-surgery they provided medications that helped to manage pain and aid sleep during the first few days of recovery.
Active Role in Mitigating Obstruction Risk
After my small bowel obstruction experience I committed to having a more active role in my nutrition in an effort to reduce obstruction risk. I began ~daily circadian fasts, primarily to confirm I was obstruction-free 🚽 prior to consuming any solid food.
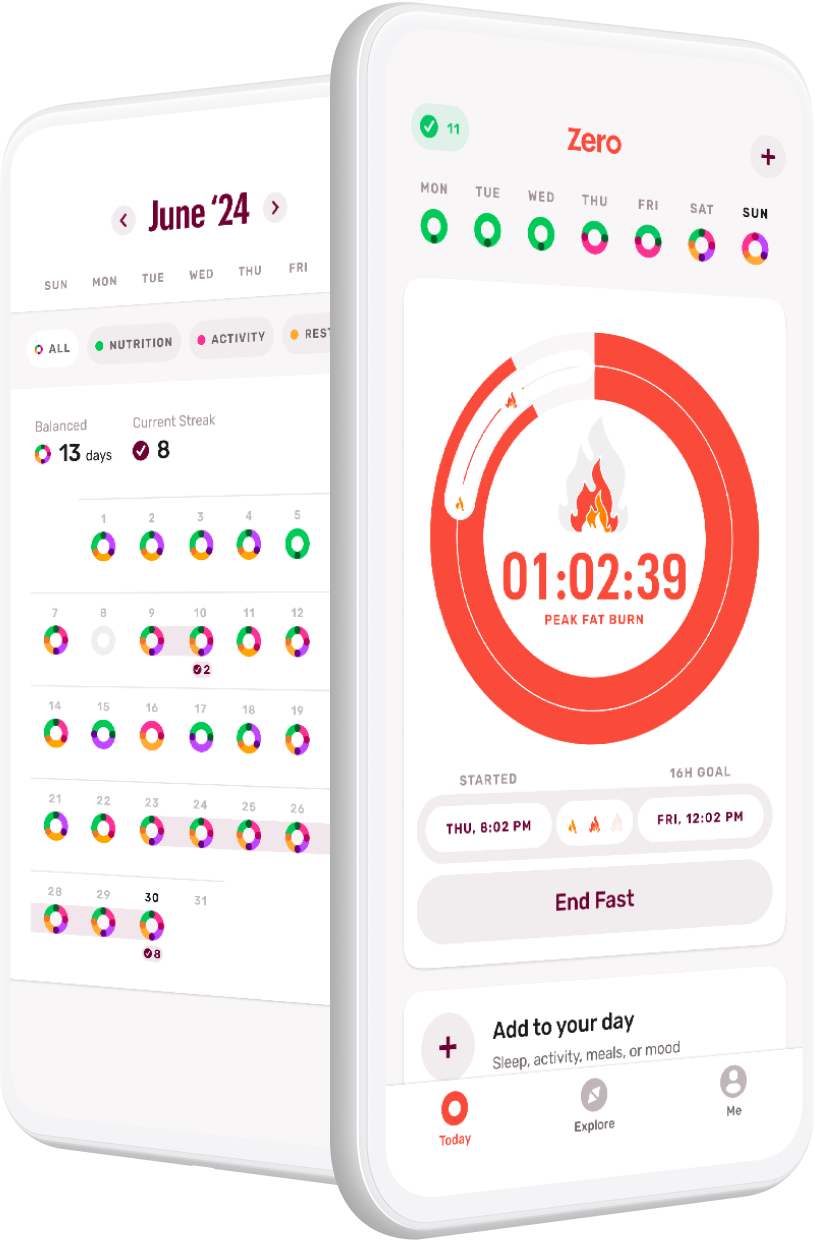
My coursework and research in graduate school revolved around exercise and nutrition. It did not take long before I invested significant time and effort into learning more about IF and time restricted feeding. I tested out consistent 16:8 TRF and found that I enjoyed it a great deal. TRF gave me an active role in my own health challenges and hospital risk equation. I believe TRF gave me control over an area of my health where I previously felt powerless. I came to IF/TRF for health reasons and I have not looked back since. I have experienced many other benefits including nutritional consistency, body composition, and unlocked time productivity that my original motivation to “avoid the hospital” seems secondary.
Fasting Experience of “Skills”
Compared with my habits in 2016 I believe my fasting “skills” have improved dramatically. When I first began fasting, 16:8 TRF was a significant challenge and I used bulletproof coffee and small non-insulinogenic Calorie inputs to consistently hit the 16 hour target. Now I easily cruise through 16 hours and frequently make it to 20 or 21 hours without even realizing that I’m still fasting. If I were to tell my pre-2015 self that in a few years daily TRF would be my “normal” and that it included often easily cruising through fasts nearing 24 hours, my pre-2015 reaction would be LOL. I consider my fasts to be “real” fasts now that they truly meet the requirement of Calorie abstinence, not that there’s anything wrong with adding some dietary support here and there if it helps you make it to your goal(s)! It took me some time to get comfortable and establish sustainable TRF habits with zero Calorie inputs. I love the flexibility and the freedom that is associated with being able to strategically select my meal time(s) rather than having it somewhat dictated to me by my body’s Calorie/carbohydrate dependency.
Fasting “Novelty” Behaviors
My guess is I am not the only one that initially used fasting to justify some poor nutritional behaviors. For the first year (give or take) the novelty of fasting provided some misguided motivation to exploit my fast breaker meal in unhealthy ways. My favorite “tradition” was to leverage fasts in conjunction with exercise to justify visits to lunch buffets with friends where we competed to see who could consume maximum Calories. Luckily, this only happened once. Per week..
My understanding of fasting and the benefits of dialing in nutrition during the eating window to support fasting benefits has matured! I rarely feel compelled to participate in these “festivals of fueling” as I did before. Instead, I get much more enjoyment developing my skills to decipher genuine signals of hunger versus those of boredom or task-avoidance. I am equally excited to break my daily fasts with a nutritious meal. I imagine many of my cells have had time to relax, organize, and clean up, therefore they are primed to use nutrients more effectively in building and maintaining health than they might be otherwise in a chronically fed/overfed state.
Morphing Motivations
My motivations for fasting have changed somewhat over the years. I am definitely not planning to do any more hospital “fasts” if I can help it. I no longer use fasting as a recurring excuse to inhale an entire all-you-can-eat buffet at least not routinely. Every now and then I relish the opportunity to throw down, especially if the buffet includes Chinese food.
I believe there is an increased margin for error associated with TRF that is missing from some other dietary patterns where you have to manipulate macronutrients or restrict Calories exclusively. I like that TRF helps me regulate body composition and health goals without reliance on calorie counting, food weighing, and/or diet tracking. Nobody is perfect and I believe TRF makes room for reasonable human error quite well relative to other diet patterns.
For example, if I choose to over-indulge I can pull on the time-restriction lever a bit more before and/or after my questionable meal. I believe the signaling clarity helps a TON for me, both psychologically and metabolically. Rather than using a strategy of Calorie restriction which would include having a smaller meal at some point during my day to compensate, I can increase my fast duration and experience greater enjoyment + gratitude during my cheat meal. Previous attempts at Calorie restriction ALWAYS results in more hunger and inevitably the strategy falls apart, in my experience; yours may be different!
Fasting Benefits
It is hard to say with certainty if IF has kept me out of the hospital during the last 6 years. I believe that it has definitely reduced my hospitalization and obstruction risks. Between 2015 and 2021 through many iterations and changing life circumstances I have been able to maintain TRF and I have noticed enhanced productivity, metabolic flexibility, body composition, and general health. Back in 2016 I was not unhealthy by any metrics, but I don’t think that I was regularly prioritizing habits that can be classified as metabolic health investments. I fast because I enjoy a range of additional benefits that extend well past my original desire to avoid hospitalization. I believe fasting is a great tool for training to improve metabolic health just as exercise is a tool for training and improving your physical body.
About the Author: Rich LaFounatin
Rich LaFountain is a science writer with a passion for exploring human health through lifestyle inputs, nutrition, and exercise. Rich completed his Bachelor of Science in Biology at The College at Brockport. He received his Master’s and Doctorate degrees in Kinesiology from The Ohio State University. He is fascinated by the manipulation of dietary patterns including fasting, macronutrient composition, and calorie restriction for targeted individualized outcomes in human health and performance.

Download Zero on iOS and Android.
- Debunking 3 Myths Around Fasting and Thyroid Health - April 15, 2024
- Breaking Down Fast Breakers: How to Tell If Something Will Break Your Fast - March 4, 2024
- GLP-1s and Weight-Loss Medications vs. Lifestyle Interventions: What’s Right for You - February 5, 2024